Opioid Overdose, Withdrawal and Treatment
An opioid overdose occurs when opioids adversely affect the part of the brain that controls respiration. This usually stems from addiction that requires detox. A dangerous and life-threatening symptom of an opioid overdose is problematic or suppressed breathing.
Without sufficient oxygen, death can occur quickly. Thus, an opioid overdose is a medical emergency that requires specific medication and medical attention immediately.
What is An Opioid Overdose?
An opioid overdose happens when high levels of opioids or opioids and other substances excessively stimulate the area of the brain controlling breathing. Respiratory depression leads to death if not treated immediately. Cardiac arrest (heart attack) is a secondary concern after respiratory depression.
Opioids are central nervous system depressants and can lead to overdose, especially when combined with benzodiazepines. Everyone has a personal tolerance level for opioids, but in many cases, people are not aware that opioids are present in the drugs they are using.
When an overdose occurs, medical professionals recommend entering a detox program immediately to avoid future overdose dangers. After an initial overdose, subsequent overdose danger increases. Treatment centers that specialize in detox are fully aware of these dangers and recommend medical supervision during detox.
The leading medication-assisted treatment (MAT) for opioid withdrawal symptoms during detox are the following:
- Naltrexone blocks the effects of opioids
- Methadone reduces withdrawal symptoms and cravings
- Buprenorphine softens withdrawal symptoms and cravings
Opioid Statistics
The Centers for Disease Control and Prevention states that in 2021, just over 50 million people in the United States reported chronic pain, and another 17 million had high-impact pain. Treatments for this population also included 139,523,956 prescriptions for opioids. In the same year, prescriptions of Naloxone exceeded 1,184,612 to treat opioid overdose, and 16,105,318 prescriptions of buprenorphine to treat opioid addiction.
The use of fentanyl in nonmedical opioids is the primary cause of the increase in overdose. Overdose is the leading cause of death in the US, with opioids at the top of the scale of use. The alarming numbers the CDC collects point to 75% of opioid overdoses stemming from nonmedical use of synthetic opioids, such as fentanyl.
Fentanyl is 50 to 100 times stronger than morphine. Illegal synthetic opioids and drug manufacturers add fentanyl to make their drugs more attractive because of the added potency. The National Institute on Drug Abuse reports in 2021, there were 80, 411 deaths from opioid overdoses.
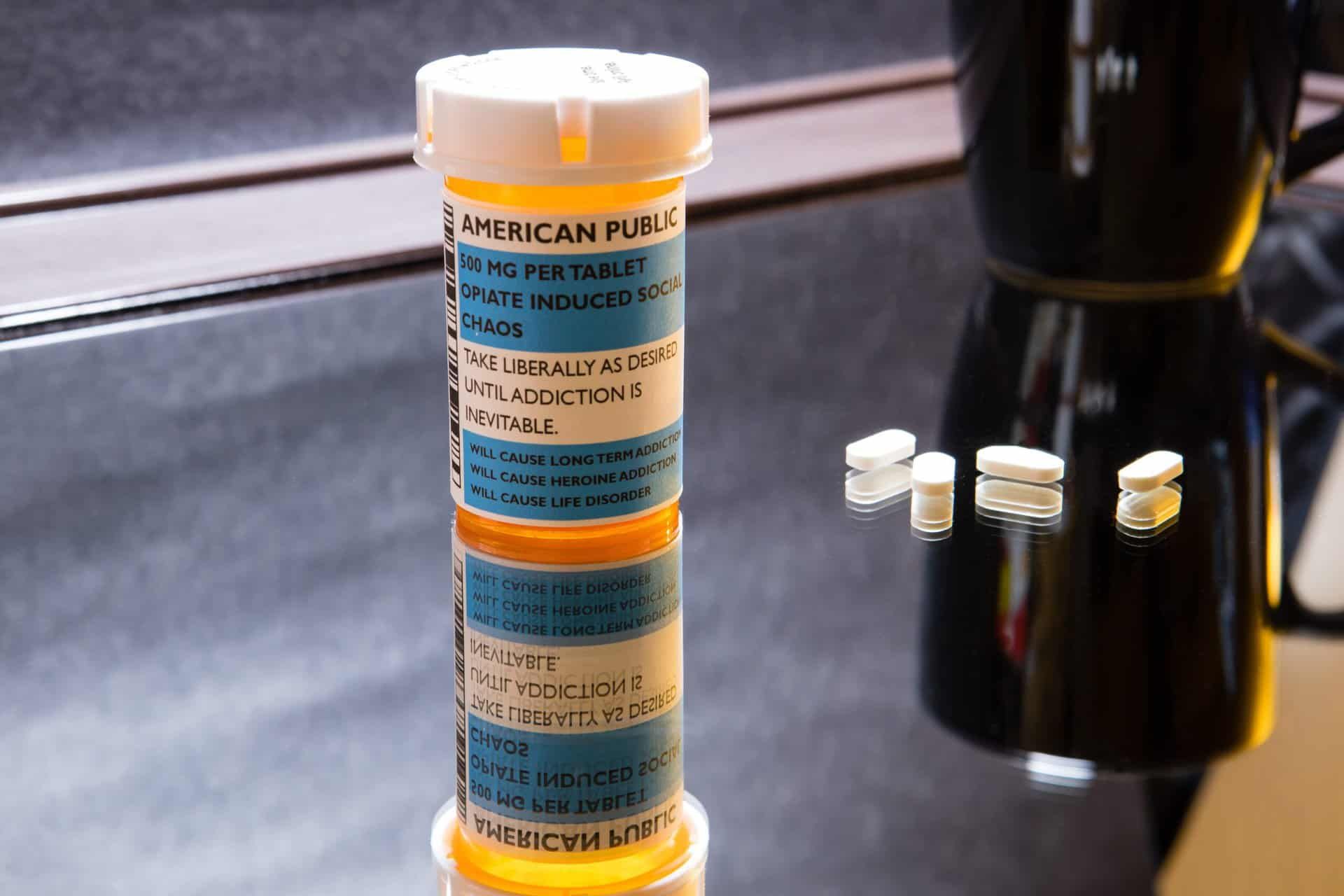
The Opioid Epidemic
An alarming trend brought opioids to the forefront when, from 1999 to 2021, nearly 645,000 people died from drug overdoses involving both prescription and illicit opioids. The Centers for Disease Control and Prevention immediately took action to monitor this horrific rise inopioid overdose deaths. In 2021, the CDC reported 220 people each day died from opioid-involved overdose.
The opioid epidemic presents in 3 distinctive waves:
- An increase in opioid prescriptions in the 1990s began the rise in opioid overdose deaths in 1999.
- In the year 2010, additional increases in overdose deaths were due to the use of heroin.
- The third and most alarming wave began in 2013 when illicit fentanyl found its way into heroin, counterfeit pills, and cocaine.
Types of Opioids
Opioids are narcotic medications that are both natural and synthetic. They can be very dangerous in their natural, purified, and concentrated form. Prescription narcotics treat chronic pain from injuries or surgery.
Opioids, primarily made in labs, are highly addictive and, through misuse, can cause unintentional addiction. Despite the dangers of addiction, opioids are the leading treatment for chronic pain.
- Hydrocodone
- Hydromorphone
- Oxycodone
- Oxymorphone
- Morphine
- Codeine
- Fentanyl
Fatal and Non-Fatal Opioid Overdoses
Non-fatal opioid overdose is much more common than fatal overdose involving opioids. Treatment options have become much more available to the public for the immediate treatment of opioid overdose. With public education on fentanyl and opioid overdose and the release of Narcan availability, fatalities are beginning to decrease. Knowing the signs of opioid overdose is essential for everyone because illicit opioid users will likely experience overdose.
The World Health Organization describes the likelihood of fatal overdose depending on the administration, with injection being more likely. Other factors that result in a higher risk of fatal overdose with opioids are if tolerance is affected by a period of abstinence. People who are in relapse, hospital care, or custody may be impacted by overdose when use begins as the tolerance level changes. An opioid overdose is always a medical emergency.
The signs and symptoms of opioid overdose include:
- Unresponsiveness or unconsciousness
- Cyanosis (blue lips or fingernails)
- Shallow, slowed or stopped breathing
- Pinpoint pupils
- Snoring or gurgling sounds coming from the mouth
- Cold and clammy skin
Opioids and Opiates: Are They the Same?
The 2 words are typically interchangeable, but they are different. Opioids are natural, synthetic, or semi-synthetic chemicals that interact with opioid receptors on nerve cells in the body and brain.
The primary function of these drugs is to reduce pain levels and feelings of pain. Opiates are natural opioids such as heroin, morphine, and codeine. Opioids refer to all-natural, semi-synthetic, and synthetic opioids like fentanyl, Vicodin, and Percocet.
Medications and Sprays Used to Treat Opioid Overdoses
Naloxone (Narcan) is the leading treatment for opioid overdose. Narcan reverses opioid overdose by being an opioid antagonist. This mediation attaches to the opioid receptors in the body and blocks the effects of opioids.
It comes in spray or injection form. The effectiveness continues for roughly 30 to 90 minutes, in time to receive professional medical treatment at a facility. Overdose effects can extend beyond that time, but physicians can address breathing issues and offer medical care.
Get Hands-On Opioid Support in Tennessee
Freeman Recovery Center, nestled in Nashville, Tennessee, offers comprehensive rehabilitation services meticulously tailored to address a wide spectrum of substance use disorders including opioid use disorder. Our specialized opioid and drug rehab programs cater to individuals battling alcohol addiction, drug addiction, cocaine addiction, heroin addiction, meth addiction, benzo addiction, and prescription drug addiction. By combining evidence-based practices with holistic care, we deliver empathetic and professional support that focuses on the unique needs of each patient. Our goal is to create a nurturing environment where teenagers and their parents feel encouraged and empowered to overcome addiction, achieve lasting recovery, and rebuild their lives with confidence and resilience.
Opioid addiction is frightening because of the chance of a fatal overdose. Freeman Recovery Center in Tennessee understands the addictive quality of opioids and how quickly tolerance, dependence, and addiction can happen. Opioid detox can be safe with medical management and the assistance of medication.
Contact the center to discuss the details of admission and begin the ending of an opioid addiction.